Copilots Arriving: Improving Claim-Related Communication and Satisfaction in Health Plan Call Centers
By Akshay Sharma, Chief AI Officer at Lyric, and Steve Ambrose, Director, Thought Leadership, at Lyric
In the intricate maze of healthcare administration, where complexity and cost often hinder efficiency and clarity, a revolution looms on the horizon. AI-driven copilots, powered by advanced small language models (SLMs), are set to transform the landscape of health plan call centers.
These technological innovators offer more than just significant cost reductions; they promise a fundamental shift towards diminishing provider friction, amplifying transparency, and streamlining financial interactions in healthcare.
As we explore this transformative journey, the role of feedback loops and personalized AI interventions marks the dawn of a new era in patient-centric and efficient healthcare administration.
The Burden of Administrative Costs: A Call for Change
McKinsey estimates that nearly 25% of total healthcare spend is attributed to administrative-related costs. In 2019 dollars, as shown below, that was $950 billion; and by 2027, it’s set to rise to $1.75 trillion per year. Extrapolating the 9% of spending for private payers—specific to customer and patient services—we’re looking at $25 billion per year and rising.
Given the volume of interactions, the complexity of healthcare policies, and the intricate nature of services, there's an undeniable urgency for innovative solutions.
The Satisfaction Slip: Addressing Call Center Pain Points
Health plan call centers are currently navigating turbulent waters as they grapple with a marked year-over-year decline in member trust and satisfaction. The latest figures from the J.D. Power 2023 U.S. Commercial Member Health Plan Study, which surveyed over 35,000 plan members across 142 plans in 22 regions, paint a stark picture: overall satisfaction has plummeted by 13 points on a 1,000-point scale. This downtrend is spearheaded by a significant 33-point drop in customer service contentment, with other areas such as coverage and benefits (-20 points), provider choice (-16), and information and communication (-16) also experiencing considerable declines.
Moreover, the Net Promoter Score® for new members is alarmingly low at 6, in stark contrast to a more moderate 25 for established members, underscoring the critical nature of onboarding processes. Compounding these challenges is the underutilization of digital health tools, with member usage not crossing the 50% threshold, signaling a disconnect between technological investment and member engagement.
In parallel, regarding growing provider abrasion, a Forrester study spotlighting provider leaders reveals over half concurring that delays in claims and payment processing are detrimentally impacting their operations, with a resounding 80% asserting that enhancements in these areas are important, if not mission-critical, for their success. This sentiment is echoed in their concerted efforts to alleviate patient burden concerning claims processing, with 78% of providers prioritizing this goal. Furthermore, 85% are actively seeking to implement payment systems that align with both patient experience aspirations and pragmatic business requirements.
These findings underscore the necessity for health plan call centers to not only streamline their operational framework but also to innovate proactively, ensuring they meet the evolving demands of both providers and plan members in a landscape where every interaction counts towards building trust and satisfaction.
Lyric’s CoPilot for Smoother Health Plan Service Journeys
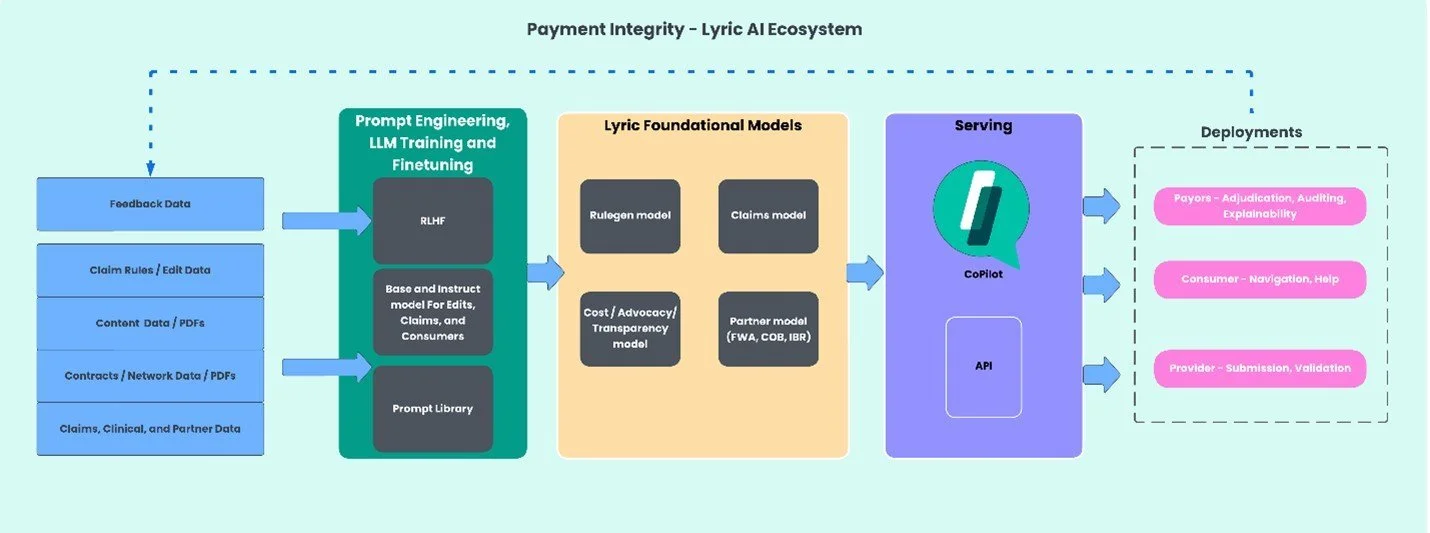
In the complex world of healthcare, where navigating the specifics of claim adjudication often presents a significant challenge, Lyric’s CoPilot represents a pivotal shift towards clarity and comprehension. With a solid foundation built on more than three decades of clinical content expertise, Lyric has developed an intricate system that leverages AI and Large Language Model (LLM) technologies. This system intricately processes claim edits, rules, regulations, and policies from a wide range of sources, including CMS, state Medicaid, and beyond, transforming them into accessible primary and secondary edits along with a suite of pre-pay claim capabilities.
When a call center receives an inquiry from a health provider or plan member, the process of demystifying claim adjudication starts with a simple yet effective query. Customer Service Representatives (CSRs), acting as the link between complex data and the inquirer, utilize Lyric’s secure data platform to access the needed information. The heart of this process is Lyric's knowledge graph, which turns dense technical data into understandable insights. This graph, a complex network of concepts, entities, relationships, and events linked through semantic metadata, ensures that the information not only is accurate but also contextualized to facilitate comprehension.
Illustrated in our discussion, this streamlined journey from question to clarity is made possible by Lyric's CoPilot. CSRs can easily navigate through the system to provide precise, easily understood explanations of adjudication queries. This clarity is soon to be extended through the integration with Interactive Voice Response (IVR) and chatbot technologies, broadening the accessibility and reach of this crucial service.
The backbone of Lyric’s CoPilot is its unparalleled commitment to keeping pace with the ever-changing landscape of healthcare governance and policy. It synthesizes an array of public and proprietary data, enriched by insights from an extensive collection of content sources. This includes detailed guidelines from CMS, specific Medicaid and Medicare information, and inputs from over 27 other critical sources, all processed through the CoPilot’s sophisticated knowledge graph. This integration of various coding systems and regulatory insights ensures that the CoPilot’s outputs are not just informed but deeply reflective of the current healthcare environment.
Lyric's CoPilot is not just a technological advancement; it’s a step towards making healthcare information more accessible and understandable for those who navigate its complexities daily. It stands as a crucial development in bridging the gap between intricate healthcare data and the need for clear, actionable information, marking a significant improvement in the way health plan call centers operate and serve both providers and members.
CoPilot in Action: Provider Inquiry on Denied Claim
Here is an example of how Lyric Copilot can assist a customer service representative (CSR) in addressing a question from a billing administrator from a provider organization. Rejections often involve technical reasons that involve heavy amounts of complexity, subject matter expertise, and a clear understanding of the underlying cause. This depth of knowledge regarding CMS rules and guidelines is not readily accessible for, and well-understood by CSRs today.
To the left, CoPilot swiftly retrieves the claim, identifies the technical reason for rejection, and provides it to the CSR. However, the technical explanation still does not reduce complexity and improve understanding—both for the CSR and the inquiring party. In such cases, the CSR can query the Lyric CoPilot and ask for a simpler explanation, as demonstrated above.
Improved Understanding, Better Communication, Increased Efficiency, and Improved Stakeholder Relationships
The introduction of a copilot, utilizing Lyric's Large Language Model (LLM), represents a significant advancement in health claim adjudication, benefiting health plan call center and provider representatives alike. This AI-driven tool simplifies complex adjudication codes, enhancing understanding and communication, and streamlining processes for improved efficiency and stakeholder satisfaction.
For CSRs, the copilot offers a clearer grasp of claim decisions, automating the translation of complex codes into layman's terms. This not only boosts efficiency and call handling but also increases job satisfaction by reducing the stress associated with explaining complicated adjudication decisions. Additionally, it serves as a continuous learning tool, enhancing staff expertise and easing the learning curve for new hires.
Provider representatives benefit from the copilot's clarity and transparency, which facilitates quicker resolutions to inquiries and allows more focus on patient care. The educational value of the copilot, offering insights into adjudication issues, helps reduce future claim rejections.
Moreover, the copilot plays a crucial role in reducing provider abrasion by streamlining communication and increasing transparency, thus fostering trust. It enables more efficient inquiry handling, enhances problem resolution, and supports stronger provider relations. By improving the quality of interactions and providing detailed, accurate responses promptly, the copilot mitigates operational friction and improves overall satisfaction.
This condensed approach underscores the transformative impact of AI in healthcare claim adjudication, promising a future of enhanced understanding, efficiency, and stakeholder relationships, underscoring the copilot's role in fostering a more collaborative and productive healthcare environment.
The Crucial Role of Feedback Loops in AI Development
The success of AI in health plan call centers heavily relies on the integration of feedback loops. These loops fine-tune the AI's performance to meet the unique needs of each customer, ensuring a tailored, personalized approach. Continuous feedback allows for the precise calibration of AI solutions, minimizing errors and aligning the technology with the specific operational needs of health plans.
Incorporating feedback into Lyric’s CoPilot is a nuanced process that ensures the AI’s continuous improvement and customization to health plan call centers. It starts with explicit feedback being obtained by prompting CSRs to give a thumbs up for effective responses, a straightforward yet powerful indicator of the AI’s performance. Absence of further questions from a caller signifies satisfaction, serving as passive affirmation of the system's efficacy.
Conversely, any indication from the CSR that the response didn’t suffice is invaluable data, signaling a need for model refinement without burdening CSRs with additional tasks.
Lyric’s approach involves a strategic deployment during a 90-day pilot where a subset of CSRs uses the CoPilot and provides feedback, mirroring the successful method applied to their content acceleration project. In this project, a dedicated team used an internal tool to assess the model’s document classification accuracy, feeding this data back into the system for enhanced learning in a controlled environment. This meticulous process of gathering and applying feedback not only sharpens the CoPilot’s accuracy but also its ability to deliver sophisticated, clear explanations.
The aim is to leverage this direct CSR feedback comprehensively during the pilot phase, allowing the CoPilot to rapidly ascend to higher levels of precision and utility in real-world settings.
Charting a New Course with AI CoPilot Innovation
The horizon of healthcare administration is brightly lit with the promise of AI-driven copilots, heralding a future where efficiency and patient-centric service are the norms. By leveraging the capabilities of small language models and integrating feedback loops, the industry can achieve unprecedented operational excellence and patient satisfaction.
This technological renaissance, while challenging, paves the path toward a future where administrative burdens are lifted, allowing providers to focus on delivering exceptional care. As we embrace this journey, the potential for transformative change in health plan call centers—and the broader healthcare system—is immense, marking the beginning of a new chapter in healthcare administration.
About Lyric
Lyric, formerly ClaimsXten, is a leading AI healthcare technology company, committed to simplifying the business of care. Over 30 years of experience, dedicated, expert teams, and top technologies help deliver up to $14 billion of annual savings to our many loyal and valued customers—including 9 of the top 10 payers across the country. Lyric’s solutions leverage the power of machine learning, AI, and predictive analytics to empower health plan payers with pathways to increased accuracy and efficiency, while maximizing value and savings. Lyric is investing in AI driven technology to ease implementation and speed to value for customer savings, while offering enhanced and newly available solutions through internal product development and strategic partnerships, including recently announced partnerships with Concert Genetics, Autonomize AI, and now, Codoxo. Discover more at Lyric.ai.